pediatric forum Winter 2018
Limb length inequality (LLI) is very common in the lower extremities. Small degrees of LLI occur in over half the population of the United States. It has been estimated that LLI of greater than 2.0 cm occurs in seven percent of the population age 8 to 12 years old. It is well known that gait patterns can be altered with discrepancies of over 2.0 cm.
Finite element models show increased sacroiliac joint loading with peak stresses increasing as the discrepancy increases from one to three centimeters, thus serving as a model demonstrating that LLI may lead to low back pain. Although no long-term studies associate osteoarthritis with limb length inequality, adults with knee osteoarthritis report pain more commonly in the short leg. Parents perceive that the happiness of their children is adversely affected by increasing limb length inequality.
etiology
There are numerous etiologies of limb length inequality that can be categorized in three general groups:
- direct change in length,
- growth inhibition and
- growth stimulation.
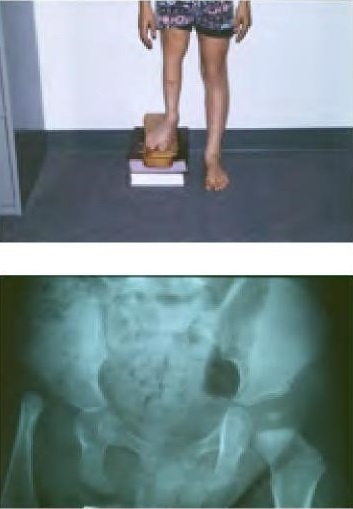
Examples of direct change in length are developmentally dislocated hips causing relative shortening of the lower extremity and fractures causing limb length inequality. Growth inhibition can be caused by numerous congenital diagnoses such as proximal femoral focal deficiency (PFFD) (Figure 1), fibular hemimelia, congenital short femur, posterior medial bowing, clubfoot or hemiatrophy. Other causes of growth inhibition include physeal injury from trauma, infection or irradiation as well as paralysis and tumors.
Growth stimulation occurs in congenital vascular malformations, vascular tumors, trauma and chronic inflammation (Figure 2).

natural history
Shapiro et al studied the natural history of LLI, publishing developmental patterns in lower extremity length discrepancies in the Journal of Bone and Joint Surgery in 1982. This landmark paper demonstrates estimated discrepancies in various conditions.
secondary effects of LLI
Gait abnormalities are dependent on the magnitude of inequality. In general, the long leg compensates by flexing the knee and circumducting or vaulting the long leg to clear the floor. The short leg compensates by standing in equinus. Energy consumption has shown to be increased secondary to significant LLI. Other secondary effects of LLI include possible increase in low back pain and association of osteoarthritis in the short leg.

evaluation
In obtaining the history, it is important to determine the etiology and if this is going to be a static or progressive deformity. Document areas of pain and disability. During the physical exam, it is essential to differentiate between a “true” LLI versus an apparent LLI secondary to joint contractures or joint instability. It is also important to perform a thorough neurologic and vascular examination (Figure 3).
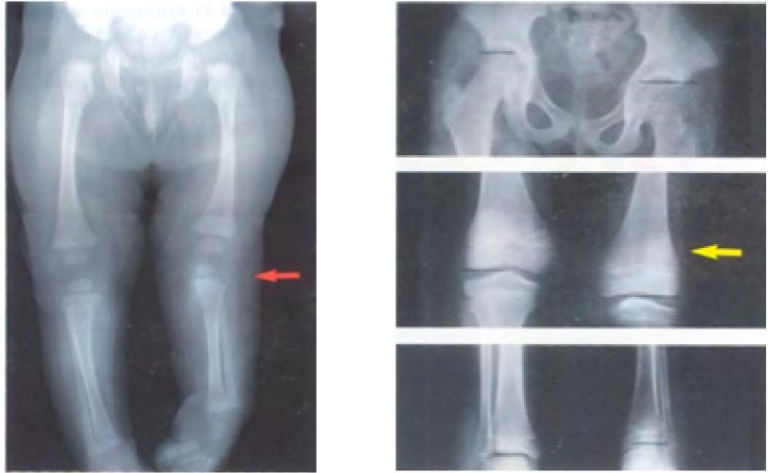
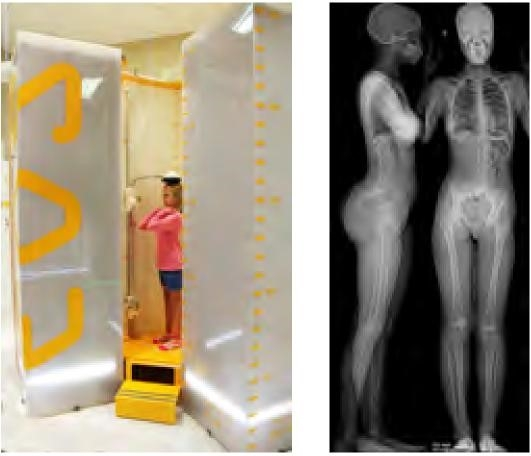
Radiographic techniques include orthoradiography (Figure 4A), scanography (Figure 4B) and computed tomography (CT). A scano-gram measures only limb lengths, whereas orthora-diograph and CT scan can measure both length and alignment. Dayton Children’s Orthopaedic Center is transitioning to low-dose radiation exposure upright biplanar radiographic imaging called EOS. This new technology allows three-dimensional imaging of the spine and lower extremities with a significant decrease in radiation exposure
(Figure 4C).
management principles
Treatment decisions about limb equalization are based on the projected limb length discrepancy at maturity. There are numerous methods to predict discrepancy at skeletal maturity. The Arithmetic Method uses the rate of growth of the distal femur (1.0 cm/year) and proximal tibia (0.6 cm/year) with growth ending at maturity in boys at age 16 and girls at age 14.
Discrepancies 2.0 cm or less can be treated with observation or shoe lift. Discrepancies from
The Growth Remaining Method uses growth remaining graphs and skeletal age, while the Straight Line Graph Method simplifies the Growth Remaining Method. Finally, the Multiplier Method uses several limb length databases and chronologic age. Sander’s Digital Skeletal Age has shown to be superior to using chronologic age in the Multiplier Method.
2 to 5 cm can be treated with epiphysiodesis prior to maturity or femoral/ tibial shortening after maturity. Limb lengthening is reserved for discrepancies over 5 cm in length. Patients with severe limb length inequality of over 20 cm with poor functioning joints who cannot tolerate limb lengthening are candidates for amputation and prosthetic fitting.
The above are general guidelines used in clinical decision making for treatment of limb length inequality. Many other factors should be considered such as overall stature, joint stability, joint contractures, neurovascular problems, and emotional stability of patient and family before undergoing limb lengthening.
state-of-the-art treatment methods
Dayton Children’s Orthopaedic Center has been at the forefront of limb deformity correction, having done the first Ilizarov Distraction Osteogenesis Limb Lengthening procedure on a child in our region in 1989.
Since then, there have been numerous innovations in circular external fixator limb lengthening devices. Most recently, we have performed the first magnetic limb lengthening using the PRECICE nail in our region. This is an intramedullary rod that has a magnetic actuator drive that uses an external electromagnetic actuator to control rate and direction of lengthening, thus eliminating the need of external fixation (Figure 5).

case study: distraction osteogenesis
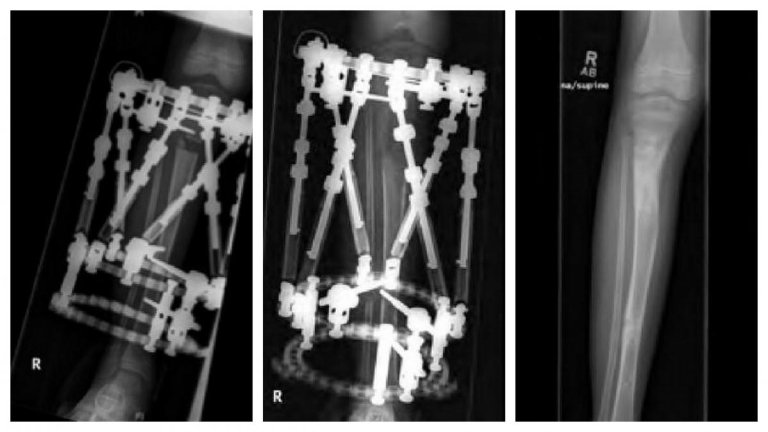
S.D. is a 2-year-old female who presented to the Orthopaedic Center at Dayton Children’s for an LLI noticed by the family. Her birth and developmental history were unremarkable and there was no family history of limb deformity. Examination revealed an LLI by tape measure and blocks of 2.5 cm left longer than right. She had hyperpigmentation involving her trunk, abdomen and left leg. Her neurovascular exam was normal, and she had hemi-hyper-trophy on her left calf with 2.5 cm increase in growth compared to the contralateral leg. A scanogram was obtained which showed a 3 cm overall limb length inequality with 2.0 cm difference in the tibias. Genetics was consulted verifying diagnosis of Klippel-Trenaunay-Weber syndrome. MRI of her brain and cervical, thoracic lumbar spine revealed no abnormalities. By age 6, her exam revealed a progressive discrepancy showing a 7.0 cm LLI; thus she had her first limb lengthening using a spatial frame external fixator and obtaining 5 cm of length, 20 percent of the length of her tibia (Figure 6).
During her lengthening of the tibia, she developed an equinus contracture on the lengthened leg requiring a percutaneous heel cord lengthening upon removal of the frame.
Despite a 5.0 cm lengthening, her LLI continued to progress and by age 10 years, 2 months, she had a discrepancy of 8.0 cm. We then did a PRECICE Femoral Nail, lengthening her magnetically an additional 6.0 cm (Figure 7).
She has regained full motion and function from her intramedullary limb lengthening having lengthened her right leg a total of 11.0 cm. We used a combination of two limb lengthening techniques, using an external fixation done on her tibia thus avoiding her growth plates. Magnetic intra-medullary lengthening can only be used in children over 10 years as the width and length of the rods are limiting factors.

conclusion
Limb length discrepancy is very common. It is important to determine the etiology and predict the discrepancy at maturity in order to determine best treatment options. Limb lengthening continues to evolve with game-changing technology on the horizon.
references
- Drnach M, Kreger A, Corliss C, Kocher D. Limb length discrepancies among 7- to 12-year-old children who are developing typically. Pediatr Phys Ther. 2012;24(4):334-337.
- Kiapour A, Abdelgawad AA, Goel VK, Souccar A, Terai T, Ebraheim NA. Relationship between limb length discrepancy and load distribution across the sacroiliac joint: A finite element study. J Orthop Res. 2012;30(10):1577-1580.
- Noll DR. Leg length discrepancy and osteoarthriticknee pain in the elderly: An observational study. J Am Osteopath Assoc. 2013;113(9):670-678.
- Lee KM, Chung CY, Gwon DK, et al. Parental perspectives on leg length discrepancy. J Pediatr Orthop B. 2012;21(2):146-149.
- Neelly K, Wallmann HW, Backus CJ. Validity of measuring leg length with a tape measure compared to computed tomography scan. Physiother Theory Pract. 2013;29(6):487-492.
- Khakharia S, Bigman D, Fragomen AT, Pavlov H, Rosbruch SR. Comparison of PACS and hard-copy 51 inch radiographs for measuring leg length and deformity. Clin Orthop Rela Res. 2011;469(1):244-250.
- Aaron A, Weinstein D, Thickman D, Eilert R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J Bone Joint Surg Am. 1992;74(6):897-902.
- Escott BG, Ravi B, Weathermon AC, et al. EOS low-dose radiography: A reliable and accurate upright assessment of lower-limb lengths. J Bone Joint Surg Am. 2013;95(23):e1831-e1837.
- Westh RN, Menelaus MB. A simple calculation for the timing of epiphyseal arrest: A further report. J Bone Joint Surg Br. 1981;63(1):117-119.
- Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45:1-14.< >Moseley CF. A straight-line graph for leg-length discrepancies. J Bone Joint Surg Am. 1977;59(2): 174-179.
- Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82(10):1432-1446.
- Sanders JO, Howell J, Qiu X. Comparison of the Paley method using chronological age with use of skeletal maturity for predicting mature limb length in children. J Bone Joint Surg Am. 2011;93(11): 1051-1056.
- Canale ST, Christian, CA. Techniques for epiph-ysiodesis about the knee. Clin Orthop Relat Res. 1990;255:81-85.
- Horn J, Gunderson RB, Wensaas A, Steen H. Per-cutaneous epiphysiodesis in the proximal tibia by a single-portal approach: Evaluation by radiosteromet-ric analysis. J Child Orthop. 2013;7(4):295-300.
- Stewart D, Cheema A, Szalay EA. Dual 8-plate technique is not as effective as ablation for epiphysiodesis about the knee. J Pediatr Orthop. 2013;33(9):843-846.
- Ilharreborde B, Gaumetou E, Souchet P, et al. Efficacy and late complications of percutaneous epiphys-iodesis with transphyseal screws. J Bone Joint Surg Br. 2012;94(2):270-275.
- Hasler CC, Krieg AH. Current concepts of leg lengthening. J Child Orthop. 2012;6(2):89-104.
- Oostenbroek HJ, Brand R, van Roermund PM, Cas-telein RM. Paediatric lower limb deformity correction using the Ilizarov technique: A statistical analysis of factors affecting the complication rate. J Pediatr Orthop B. 2014;23(1):26-31.
- Rozbruch SR, Birch JG, Dahl MT, Herzenberg JE. Motorized intramedullary nail for management of limb length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22(7):403-409.
earn CMEs
This article is part of a recent issue of Pediatric Forum, a journal for physicians by physicians. To explore this issue and past issues and for a chance to earn CME credits, please use the link below.
care that goes above and beyond
Because every child deserves care that goes above and beyond, Dayton Children’s provides compassionate, expert care for kids of all ages. Find a provider, schedule an appointment, or learn more about conditions we treat today.
