pediatric emergency medicine fellowship
Advance your career in pediatric emergency medicine through individualized, hands-on training that builds clinical expertise, leadership and research excellence.
why choose a Dayton Children’s fellowship?
The pediatric emergency medicine (PEM) fellowship at Dayton Children’s Hospital, in affiliation with Wright State University Boonshoft School of Medicine, provides rigorous, individualized training that prepares fellows to excel as clinicians, educators and researchers.
As the region’s only verified Level I Pediatric Trauma Center, Dayton Children’s offers an unparalleled learning environment where fellows manage high-acuity cases alongside experienced pediatric emergency physicians, trauma surgeons and critical care specialists. This hands-on experience helps fellows build the confidence and clinical judgment needed to care for children in any emergency situation.
Each fellow follows a personalized curriculum designed to advance clinical skills, research interests and leadership development. Supported by dedicated faculty mentors and a culture of innovation, fellows are encouraged to pursue meaningful scholarly work that contributes to the advancement of pediatric emergency care.
Dayton Children’s combines academic excellence with compassion, teamwork and a shared commitment to improving outcomes for kids.

locally focused, nationally recognized
While our pediatric experts are nationally recognized, it’s our specialty in caring for kids locally that truly sets us apart. No one is more committed to the health and wellbeing of the children of our community than Dayton Children’s – and that includes providing support, training and development to the future in pediatric hospitalists.




related resources
follow our PEM fellowship on Instagram
learn morePEM fellowship program details
learn moreresearch & innovation at Dayton Children’s
learn morewhy families choose Dayton Children’s
learn moremeet our program leadership team
Get to know the pediatric emergency medicine fellowship program leadership who will support and guide you during your fellowship. Our faculty are leaders in pediatric emergency medicine, dedicated to advancing your skills and passion for exceptional patient care.

Richard Strait, MD
program director – pediatric emergency medicine fellowship
Additional roles:
- Associate chief, division of emergency medicine
- Medical director, Dayton Children’s emergency department – south campus
- Professor of pediatrics, Wright State University Boonshoft School of Medicine
Education and training:
- Medical School: University of Cincinnati College of Medicine
- Residency training: Cincinnati Children’s Hospital Medical Center
- Fellowship training: Cincinnati Children’s Hospital Medical Center
- Board certified in pediatrics and pediatric emergency medicine

Pradeep Padmanabhan, MD
associate program director – pediatric emergency medicine fellowship
Additional roles:
- Pediatric emergency medicine fellowship development director
- Associate professor of pediatrics, Wright State University Boonshoft School of Medicine
Education and training:
- Medical School: Stanley Medical College
- Residency training: Long Island Jewish Medical Center
- Fellowship training: University of Louisville
- Board certified in pediatrics and pediatric emergency medicine
advancing care with advanced training
The pediatric emergency medicine (PEM) fellowship at Dayton Children’s Hospital provides advanced, hands-on training in the diagnosis and management of acutely ill and injured children. The program emphasizes individualized education to support each fellow’s clinical, academic, and research goals—with a focus on achieving independent practice during the final year of training.
curriculum structure
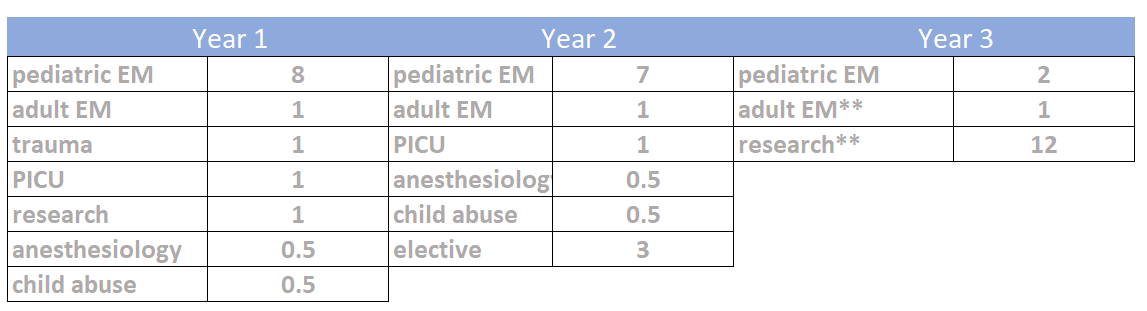
Our fellowship offers both two- and three-year training tracks depending on prior residency experience.
(For graduates of pediatric residency programs — optional third year available for emergency medicine residency graduates)
Each academic year consists of 13 blocks (28 days per block) and include the following rotations:
- Adult emergency medicine: 12 shifts distributed throughout the third year
Research: 12 dedicated research blocks in the final year - Child abuse & anesthesiology: two 2-week rotations
- Toxicology (longitudinal): 1–2-week rotation at the Drug and Poison Information Center (DPIC), monthly virtual DPIC conferences, annual zoo and botanical garden outings with the toxicologist, and toxicology journal club
- Electives are available in a variety of pediatric subspecialties including: Burn care, Cardiothoracic ICU, Developmental pediatrics, International travel medicine, Medical education, NICU and Newborn nursery, Ophthalmology, Orthopedics, Plastic surgery, Procedure, Sports medicine, Transport and EMS, Ultrasound
Every fellow receives 4 weeks of vacation time every academic calendar year. These are taken during the pediatric emergency rotation.
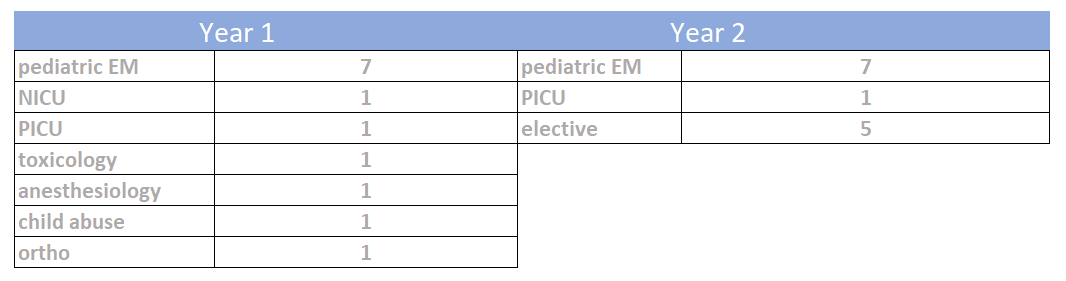
(For graduates of emergency medicine residency programs)
Each academic year consists of 13 blocks (28 days per block) with a tailored focus on pediatric emergency medicine, research, and teaching experience.
Every fellow receives 4 weeks of vacation time every academic calendar year. These are taken during the pediatric emergency rotation.
educational opportunities for fellows
Pediatric emergency medicine fellows at Dayton Children’s benefit from a rich academic environment that blends structured learning, hands-on simulation and interprofessional collaboration. Regular conferences, seminars and simulation experiences reinforce clinical decision-making and ensure fellows are well-prepared for both board certification and independent practice.
Core learning experiences include:
- Fellow-focused education: Weekly PEM fellows conference, monthly journal club, monthly research seminar, monthly trauma and radiology conferences, and quarterly PEM board reviews.
- Simulation and skills development: Monthly high-fidelity sessions in Dayton Children’s simulation lab, procedural workshops, and cadaver-based training to strengthen technical and teamwork skills.
- Collaborative academic opportunities: Participation in pediatric grand rounds, morbidity and mortality reviews, and the annual Acute Care Symposium, alongside multidisciplinary peers.
- Teaching and leadership development: Fellows serve as PALS instructors, lead simulation lab sessions for residents and students, deliver resident lectures, and present at grand rounds and annual Fellows Day—building both confidence and teaching expertise.


locations you’ll work
Throughout your pediatric emergency medicine fellowship, you’ll typically work at the following locations:
research as a PEM fellow
Pediatric emergency medicine fellows at Dayton Children’s receive comprehensive research training designed to build confidence and skill at every stage of their academic journey. Through a dedicated seminar series, fellows gain a strong foundation in study design, data analysis and scholarly writing. Certified courses in epidemiology and biostatistics at Wright State University further strengthen their evidence-based practice skills. Each fellow benefits from dedicated research funds, access to a statistician and individualized mentorship to guide project development from concept to publication. Fellows also participate in Dayton Children’s annual Fellowship Research Day, which showcases scholarly work from across subspecialty programs. We welcome candidates with all levels of research experience—including those who are new to academic investigation.
- Complete research curriculum including a lecture series on principles of research and certificate courses at Wright State University that focus on biostatistics and epidemiology
- Develop research question and plan
- Form scholarship oversight committee and select mentor
- Identify funding opportunities and apply
- Obtain IRB approval and begin research
- Present research plan within PEM division and at the National Fellows Conference
- Complete data collection and analysis
- Begin manuscript preparation
Present findings to research and oversight committees
Finalize manuscript submission
Present at regional and national scientific meetings
fellowship salary & benefits
The stipend for a fellow varies by year:
- First-year: $74,500
- Second-year: $77,800
- Third-year: $81,000
Fellows at all training levels receive 4 weeks of paid vacation annually.
All fellows have an allowance up to $5,500 for academic funds per academic year. Popular uses for these funds include:
- Board preparation
- Professional meetings
- Professional conferences
- Books and subscriptions
- Professional organization membership
Fellows receive the following insurances:
- Professional liability insurance while at Dayton Children’s and other training sites.
- Long-term disability and life insurance
- Medical, dental and vision insurance are available
Residents are appointed as junior resident instructors at Wright State University’s Boonshoft School of Medicine. This entitles the resident to faculty privileges at the university, including access to the library and athletic facilities, plus faculty discounts for software downloads and at the university bookstore.
- Free parking on-site at all locations
- Free Dayton Children’s logowear and white coat, including optional name embroidery
- On-site child care available
- Wellbeing program with many resources for all staff to support your optimal wellbeing throughout fellowship
- Access to fitness centers at Wright State University and Dayton Children’s
our emergency medicine fellows
At Dayton Children’s, we’re proud to support our pediatric emergency medicine fellows as they advance their skills and contribute to research that shapes the future of pediatric care. Below you’ll find selected publications, research projects, and honors that highlight their commitment to clinical excellence, discovery, and compassionate care.
- Padmanabhan, P., & Elliot, J. (2023). CT scans in pediatric trauma. Trauma Reports, July 2023.
- Padmanabhan, P., & Elliot, J. (2024). Scarlet fever and invasive streptococcal disease. June 2024.
- Elliott, J., Fonseca, L. D., Dereci, L., Ochoa, P., Taylor, M., & Kumar, G. (2024). Sociodemographic profile and clinical presentation of young children unintentionally exposed to marijuana: A single-site retrospective cohort. American Journal of Addiction. Advance online publication. doi:10.1111/ajad.13617
- Schissler, K., Stewart, S., Phamduy, T., Brimacombe, M., Waynik, I., & Hoppa, E. (2023). High-risk markers and infection rates in febrile infants aged 29 to 60 days presenting to an emergency department during the COVID-19 pandemic. Pediatric Emergency Care, 39(11), 895–899. doi:10.1097/PEC.0000000000002968
- Phamduy, T., Potts, E., Shareef, A., Rodeman, J., Lakeberg, J., Weisbecker, L., Forster, B., & Ziemnik, L. (in press). Reducing radiographs in low-risk infants with bronchiolitis: A quality improvement initiative. Annals of Emergency Medicine.
- Phamduy T. Where Are the Pediatricians? JAMA. 2025;333(4):349–350. doi:10.1001/jama.2024.23921
Ramgopal S, Badaki-Makun O, Eltorki M, Chaudhari P, Phamduy T, Shapiro D, Rees CA, Bergmann KR, Neuman MI, Lorenz D, Michelson KA. Trends in Respiratory Viral Testing in Pediatric Emergency Departments Following the COVID-19 Pandemic. Ann Emerg Med. 2025 Feb;85(2):111-121. doi: 10.1016/j.annemergmed.2024.08.508. Epub 2024 Oct 16. PMID: 39425713. - Eltorki M, Hall M, Ramgopal S, Chaudhari PP, Badaki-Makun O, Rees CA, Bergmann KR, Shapiro DJ, Gonzalez F, Phamduy T, Neuman MI. Trends and hospital practice variation for analgesia for children with sickle cell disease with vaso-occlusive pain episodes: An 11-year analysis. Am J Emerg Med. 2024 Dec; 86:129-134. PMID: 39427500.
- Elliott, J, Fonseca, L. D., Dereci, L., Ochoa, P., Taylor, M., & Kumar, G. (2024). Sociodemographic profile and clinical presentation of young children unintentionally exposed to marijuana: A single site retrospective cohort. The American journal on addictions, 33(6), 656–663.
- Determining the completion rate of outpatient renal and bladder ultrasound in young children following diagnosis of assumed first febrile urinary tract infection in the pediatric emergency department. Erica Potts, Shernaz Wadia
- Predictors of Emesis in Children with Ketamine Procedural Sedation. Sandhia Khatwani, Ashima Goyal
- Robert Copley Cohn Memorial Research Grant, 2024. Phamduy T, Raymer M, Banerjee T, Vacchrajani S. $40,000
- Resident & Fellow Research Support Grant Program Award, 2025. Dayton Area Graduate Medical Education Community. Phamduy T. $2,500
- Robert Copley Cohn Memorial Research Grant, 2024. Dayton Children’s Hospital Foundation, Phamduy T. $40,000
- Ayman El-Sheikh Scholars Program, 2024. Dayton Children’s Hospital Foundation. $10,000
- Fellow Research Excellence Award, 2025
- Dayton Children’s Above and Beyond: Collaboration Award, Research Education, 2025
- Edith Nourse Rogers STEM Scholarship, 2024-Present
applying for pediatric emergency medicine fellowship
Dayton Children’s Hospital and Wright State University Boonshoft School of Medicine Pediatric Emergency Medicine Fellowship will accept two fellows per year.
Only applicants who meet the following prerequisites will be considered for interviews:
- Completion of an approved general pediatric residency program or emergency medicine residency program at time of fellowship start date
- Board eligibility or certification by the American Board of Pediatrics or American Board of Emergency Medicine
- A strong interest to teach medical students, residents, and faculty
- Ability to obtain a state of Ohio medical license
- A strong history of professionalism and ethical behavior in the workplace
- Permanent U.S. residence, U.S. citizenship or green card holder
Our fellowship program will participate in the NRMP Match (ACGME program code 3243832050) and will only accept applications through ERAS.
For additional information, contact our fellowship coordinator:
Alison Moyer, MS, ATC
937-641-5279
MoyerA@childrensdayton.org
ready to take the next step?
Join a program that values your growth, challenges your skills and celebrates your calling to care for kids. Discover why Dayton Children’s is the ideal place to train, learn and lead in pediatric emergency medicine.
